
Your Explanation of Benefits (EOB) is better than ever
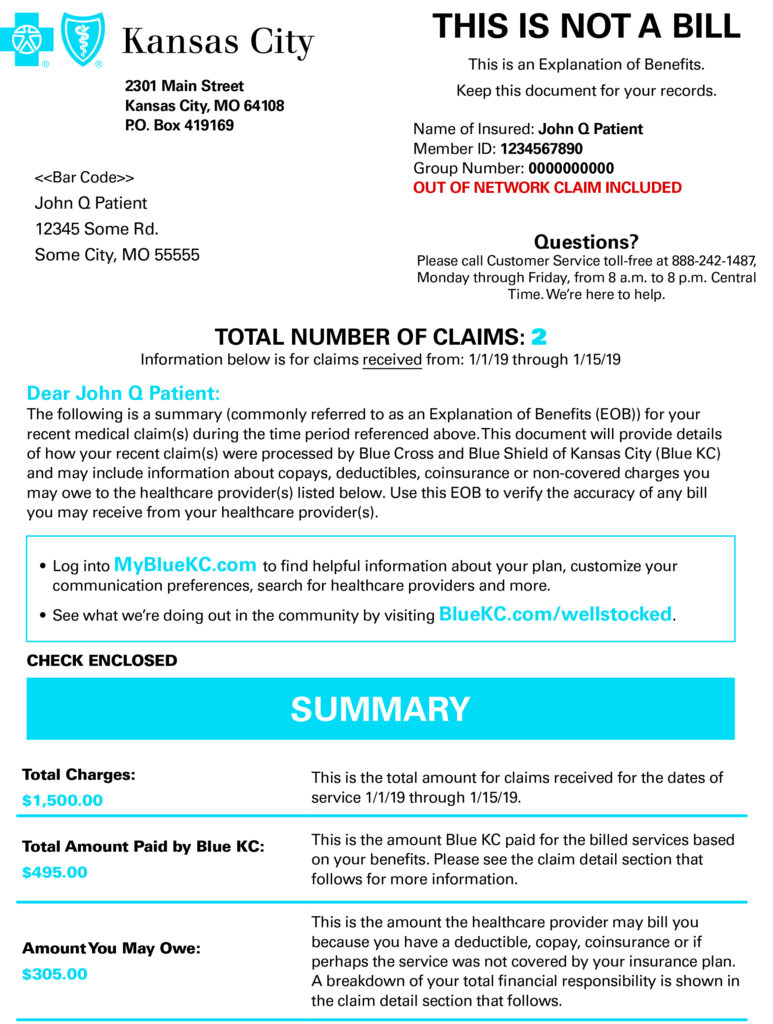
Once you visit your doctor, and have a claim with Blue KC, you receive an Explanation of Benefits (EOB). We send this statement after we process your claim. An EOB contains important terms and information – including how much money you may be responsible for paying on a claim.
EOBs are generated within approximately 14 days of a claim being processed. If multiple claims come in within the 14-day window, they’ll be included on the same EOB.
We’ve enhanced your EOBs with new user-friendly features like:
- A simplified summary and visual display providing high level details of claim(s)
- An easy-to-read, detailed breakdown of claim(s) clearly highlighting your Blue KC discount, what Blue KC is covering, your copay, and more
- A section that highlights your healthcare-related financial savings
- A simplified summary providing high level details of the claim(s)
- A detailed breakdown of each claim showing your Blue KC discount, what Blue KC is covering, your copay, and more
- A section that highlights your healthcare-related financial savings
- Deductible and maximum out-of-pocket summaries in a format similar to what you see in your member portal
Want to view your EOBs?
Remember, your EOBs are available to view in the Claims & Usage section of your member portal at MyBlueKC.com. You can also sign up for paperless EOBs by visiting your communication preference center – from there you can register to receive an email or text notification when an EOB is ready to view in your member portal.
To learn more, you can visit the Understanding Your Explanation of Benefits section of your member portal.
Have EOB questions? We have answers.
If you have questions or need assistance reviewing your EOB, please call customer service at the following number (also listed on your Blue KC member ID card). We’re available Monday through Friday from 8 a.m. to 8 p.m. CT.
If you have a Blue KC plan with access to Spira Care, call Customer Service at: 913-29-SPIRA (77472) or toll free at 1-877-33-SPIRA (77472). Otherwise, call Customer Service at 816-395-2953, or toll free at 1-866-859-3822.
