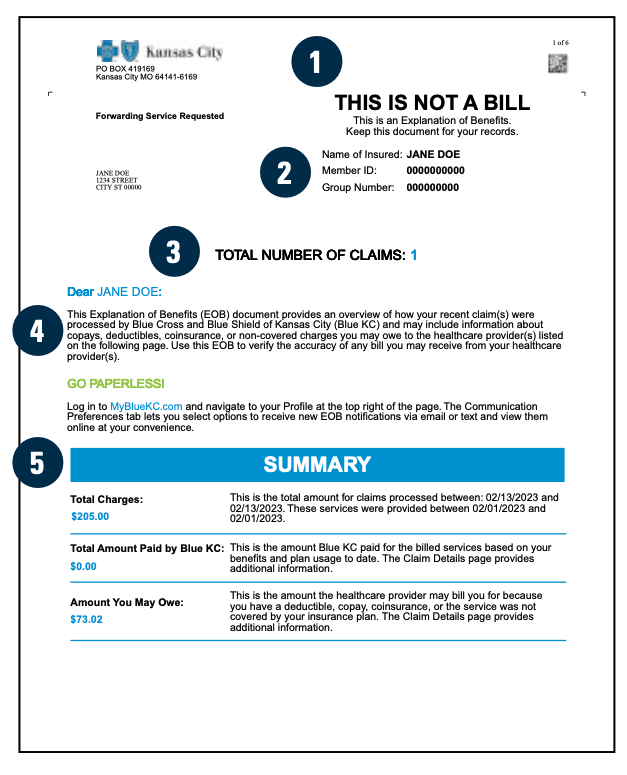
- This is Not a Bill: Your EOB is documentation of how Blue KC has processed your claim. If you do receive a bill from your provider, this is the amount you may owe. Use your EOB to verify the accuracy of any bill you may receive from your healthcare provider.
- Member Information: Information about you and your insurance coverage. If an out-of- network claim has been filed, it is noted here.
- Total Number of Claims: Information about your recent claim(s) within the time period outlined.
- Narrative: A brief overview of how your claim was processed.
- Summary: A simple overview to show how your claim is paid. Please review the Claim Details section for further details.
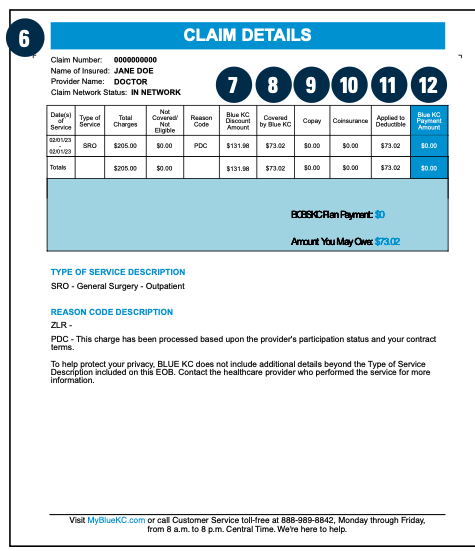
- Claim Details: This area combines critical payment information into one convenient summary. Please review this carefully as it outlines the Blue KC negotiated savings as well as any fees and services for which you are responsible.
- Blue KC Discount Amount: Blue KC has negotiated savings with providers on your behalf. Please note any out-of-network provider may bill you for an additional amount based on contract status.
- Covered by Blue KC: This is the total of the claim after all discounts and other reductions. Deductible and coinsurance amounts are calculated from this figure.
- Copay: The amount a member must pay each time a specific covered service is received, if your policy includes copayments.
- Coinsurance: The percentage of an allowable charge you must pay for a covered service. Generally, the deductible must be met before your coinsurance applies.
- Applied to Deductible: The portion of the claim being applied to your plan deductible. This amount must be paid by you before benefits become payable by Blue KC.
- Blue KC Payment Amount: This is the amount that Blue KC will pay to the provider or member for the claim.
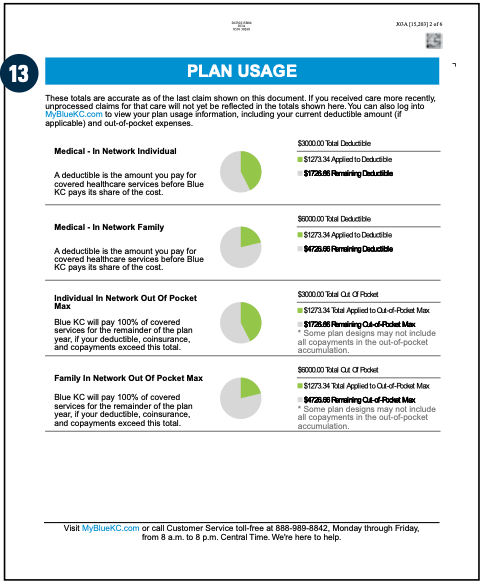
- Plan Usage: This area documents what your deductible status was at the time the claim was processed. Many times, this information will be outdated by the time you receive an EOB. You can get your most recent and up-to-date deductible information in your member account under the Claims & Usage section.